Image source: https://www.healthline.com/health-news/children-born-via-ivf-face-higher-health-risks
By Elpida Velmahos, JHBL Staff Member
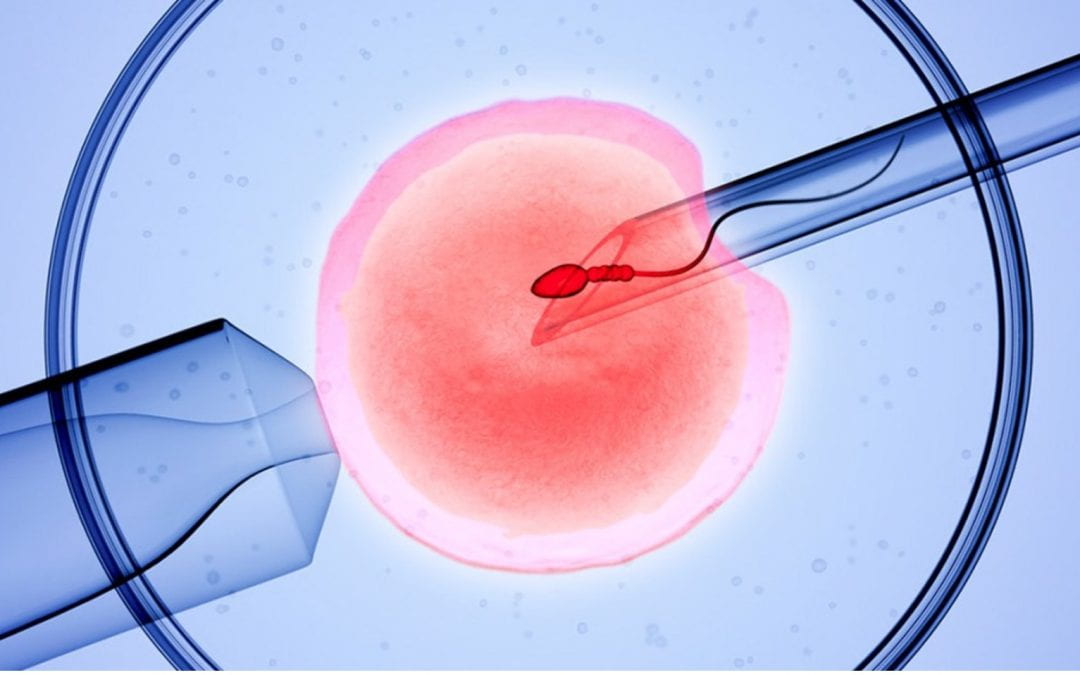
What sounds like a distant, futuristic, sci-fi invention is now a modern-day reality—creating life after death. Posthumous reproduction is a type of assisted reproductive technology (ART). ART includes In-vitro fertilization (IVF) and cryopreservation of gametes (egg and sperm) & fertilized embryos. Both address the innate human drive we possess—to survive and reproduce. New reproductive technologies allow many people to participate in the process of reproduction who otherwise, either because of personal biological hindrances or overall life circumstances, may not have been able to. Every revolutionary technological innovation, however, is followed by many ethical, legal, and social implications. These implications all need to be examined socially and legally to create appropriate policies to prevent systemic abuse, protect the interest of the innocent and unable, and maintain the balance of all interests involved. Posthumous reproduction (PHR) allows the non-coital reproduction of a child to take place using the gametes of a deceased parent (most commonly that of the biological male parent) using ART.
ART technologies first came into the medical field in the late 70s. The first test-tube baby, Louise Brown, was born in 1978 in England. Exactly twenty years later, in 1998, the first postmortem pregnancy was successfully carried out. Since then, the field of ART has grown exponentially. The current economic state and desire of couples to advance professionally before having children, has delayed pregnancy for many. While this has granted many couples more autonomy over personal, professional, and economic decisions, our flawed human biology manages to intercede. Thankfully, with technologies like IVF, couples are able to have children at older ages. Furthermore, IVF has proven to be beneficial for those with difficulties conceiving because of health reasons, as well as preventing flawed genetic traits from being passed on from parent to kin (for example, cystic fibrosis, an autosomal recessive gene, could possibly be detected in a fertilized embryo of a couple hoping to conceive and allow them and the physician to choose the healthiest embryo without a cystic fibrosis mutation). IVF has also given single parents, same-sex couples, and transgender persons the opportunity to conceive, which previously was not possible with the same level of ease. While IVF does face certain legal and ethical implications, it is easier to delineate practices and policies concerning this type of conception. The hopeful-to-be-parents are alive and able to provide their informed consent for these procedures. Furthermore, policies exist to address more special situations, like that of a single parent looking to conceive with a donor in lieu of a partner. Posthumous reproduction rides on stormier waters and is riddled by many ethical and legal considerations that make it difficult to create overarching policies which address these issues. If a couple decides to pursue IVF, their treating physician asks them two questions:
- If one of the two partners dies, is the surviving partner granted the right to use the fertilized embryo?
- If divorce ensues, can the partners use the fertilized frozen embryo?
For posthumous reproduction, the two most important types of consent are expressed – clearly and explicitly stated in writing or speech and implied consent – where a patient’s actions and circumstances of the situation allow an inference of consent to treatments mirroring the patient’s wishes. Expressed consent creates no problems; implied consent does. Two partners, “Jane” and “David,” may have privately expressed to each other the desire to produce biological children. If David passes away, Jane may desire to use his genetic material to produce a child that is biologically related to her and her late husband. However, because no expressed consent existed beforehand, Jane runs into roadblocks to legally obtain her late husband’s genetic material. In the U.S., the lack of policies on PHR creates this issue, and the lack of proper direction prevents the ease of clear decisions from being made.
Ethical Issues
Respect for autonomy – In medical care, respect of the patient to make autonomous decisions, under a sound state of mind and full information from healthcare staff is held to the highest standard. However, in the case of a deceased individual, it is much harder to determine the autonomous decisions of that person. The healthcare provider or facility, therefore, is burdened with the task of deciding whether the autonomous decision of the deceased versus that of the requestor is held to a higher priority.
Beneficence – A physician works in the best interest of the patient, but if the original patient is deceased and no explicit consent on PHR exists, then whose interest does the physician work for—the deceased or the requestor? This, in turn, burdens physicians, clinics, and the hospital with making a situational and often time-sensitive decision.
Non-maleficence- A physician’s core oath to all patients is to “do no harm.” There is much to consider under this umbrella. First, the physician must ensure that they “do no harm” to the deceased patient. The invasive nature of the gamete retrieval procedures makes it unclear whether the deceased patient and their body are being unduly violated. Extraction of gametes through sexual stimulation or removal/biopsy of genitalia rides on a thin line of bodily violation when there is no expressed consent. Second, does the physician run the risk of imposing psychological harm to the future child who will live without their biological parent? While there are certainly many children who are “produced” without the full genetic material of their legal parents, this situation differs from others in that the child is produced from the genetic material of a deceased parent (vs. a parent who used donor eggs or sperm). Thus, is it ethical to knowingly participate in bringing a child into the world under the possible pretense of psychological distress? Third, if a healthcare provider refuses the request of the widow/er spouse, are they complicit in imposing psychological harm to this person by preventing them access to the genetic material of their spouse?
Legal Issues
Gamete ownership – It is difficult to establish who the gametes belong to after the death of the male. Discussion of gamete ownership of a male is more common in PHR scenarios given the more feasible access to sperm retrieval postmortem compared to egg retrieval postmortem. One may argue that the gametes do belong to the deceased, but because reproductive tissue is not considered to be “person or property,” it becomes difficult to establish legal ownership. A counterargument for allowing a spouse to use their husband’s genetic material is equating the gamete donation to organ donation. However, these two tissues serve inherently different purposes; organs preserve life while gametes create life. While the organic body that holds the genetic material may be considered an organ (i.e., testes), the material inside is considered to be a secondary organ existing in the function of the primary. Therefore, genetic material cannot be considered solely as an organ in itself. Organ donation exists to preserve life that already exists; thus, this argument cannot be applied to create life that does not yet exist. Second, it is further difficult to establish who has the right to make the request for the gametes. Why does a partner have more authority to request genetic material versus a grandparent or sibling? What are the motives of the requestor in wanting to use these gametes for reproduction?
Inheritance rights – If a child is successfully produced through PHR, the question of inheritance comes into question. Does this child have any legal rights to the estate of the deceased? Does the child have the legal right to use government benefits, like Social Security, even though the child was produced posthumously? Some states allow inheritance if it is explicitly stated in the will, while others do not allow the PHR child to access benefits like Social Security. This also brings into question the motives of the requestor. If the requestor was in a relationship with the deceased individual and this individual had a large estate, it is a potentially valid concern that the requestor wishes to produce a genetically related child or heir to access this estate.
Currently, there are no standard laws that work with this issue in the United States. Further problematic is the continued acceleration in ART and the difficulty of governmental policies to keep up-to-pace. The American Society of Reproductive Medicine (ASRM) has the following policy: PHR is ethically justifiable if written consent exists. However, in the absence of such consent, requests should only be granted to the partner of the deceased. Furthermore, ASRM states that it is important to allow for a time period of grieving and counseling—a partner in their grieving period may wish to create a “replica” of their deceased partner so, ASRM states that it is crucial to allow for a time period to pass so the surviving partner makes a sound judgement in pursuing PHR. The European Society of Human Reproduction and Embryology (ESHRE) has a bit more of a delineated policy. Prior written consent is required if the surviving partner wishes to proceed with PHR. If the surviving partner wishes to pursue this reproductive avenue, they must undergo counseling and allow for a 1-year bereavement period. Gametes are available only to the surviving partner, and gametes/embryos must be destroyed in the event that both partners expire.
Policy recommendations
As discussed, the primary issues centered in posthumous reproduction discussions focus on the consent of all parties involved. If every person seeking PHR had explicit consent of their late partner, well, this issue obviously wouldn’t be a point of controversy! Some legal and ethical ambiguities may take longer to solve; creating a general outline will help decision-making processes and serve as precedent when trying to develop solutions to the more legal and ethically ambiguous parts of PHR. In terminal conditions, gamete retrieval should be carried out according to the hospital’s ethical committee guidelines. If there is ambiguity, the ethics committee should be contacted immediately, given that gamete retrieval is a time-sensitive issue. The requestor should be a spouse or long-term partner of the deceased. Spouse is much easier to define, while long-term is not. In defining a long-term partner, it would be helpful to consider two things, the age of the partners and the length of the relationship. Relationships between two partners of mid-age (i.e., 35-40) may be viewed differently than two partners of younger age (20-25). Therefore, it will be important to define whether one age group takes precedence over another and establish appropriate age ranges. If the deceased has not explicitly granted the estate to the PHR child, then a level of restriction would be reasonable. This would prevent spouses or partners from seeking PHR with the sole purpose of accessing their partner’s estate.
To conclude, PHR is an innovative solution that allows spouses or partners to create children that are genetically related to a deceased parent. However, in the absence of explicit consent, many ethical and legal issues arise. The U.S. lacks concrete policies surrounding this issue. There are several legal and ethical issues to consider when looking at PHR, but this should not hinder the creation of appropriate policy. Furthermore, baseline policy can help policymakers create guidelines in the future that cover the trickier legal and ethical issues surrounding PHR. Additionally, this will generate more discussion on the issue which can generate more ideas on how to approach PHR in ethical and legal ways that protect the interests and rights of all parties. As medical technologies continue to evolve, it is important that the governmental policies stay up-to-pace, representing the issues of their constituents but also creating necessary societal balances.
Elpida Velmahos is a 2L day student at Suffolk University Law School and a staff member for the Journal of Health and Biomedical Law. She graduated from Boston University (2017) with a B.S. in Human Physiology and from Columbia University (2019) with an MPH in Health Policy and Management. She has an array of interests in the health law field, such as reproductive law, healthcare reform, and food policy.
The author can be reached at evelmahos@su.suffolk.edu.
Disclaimer: The views expressed in this blog are the views of the author alone and do not represent the views of JHBL or Suffolk University Law School.
Sources:
Ahmed Elsayyad. Informed Consent for Comparative Effectiveness Trials. 370 New England Journal of Medicine 1958 (2014); doi:10.1056/NEJMc1403310.
Shane Lipskind, and Elizabeth Ginsburg. Posthumous Assisted Reproduction. UpToDate (2019) www.uptodate.com/contents/posthumous-assisted-reproduction.
https://www.cdc.gov/art/whatis.html